Friends — In our last Endemic, we covered how boosters (1st and 2nd) are effective at reducing serious illness. Thanks to recent reporting from the Washington Post, we now know we’re likely to see 2nd boosters ready in mid-September for adults under age 50. These boosters will be upgraded for Omicron variants and offer greater protection.
We also explained it’s probable most Americans won’t get the 2nd booster, partially due to decreased trust in government, medical institutions, and each other.
A recent study published in The Lancet of 177 countries found that countries with high governmental and interpersonal trust had lower levels of COVID and higher vaccination rates. So why has America’s social trust been declining and what can we do about it? We don’t claim to know all the answers, but we can make some suggestions.
📊 Washington’s COVID-19 Weekly Snapshot
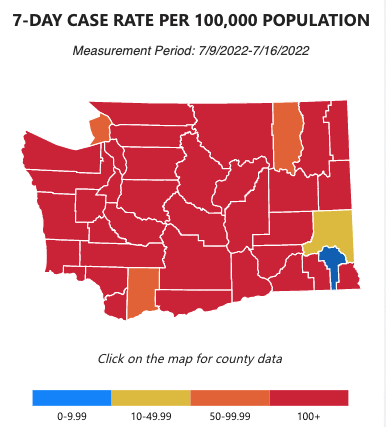
COVID cases 😷
Hospitalization rates 🏥
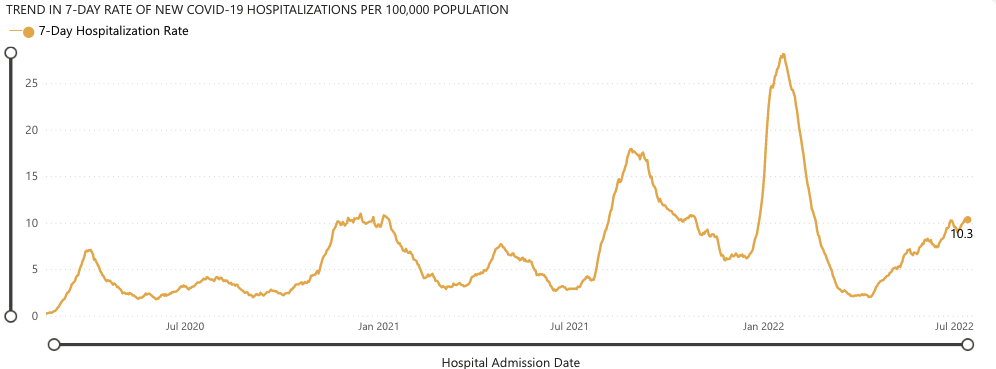
COVID’s Omicron BA.4 and BA.5 variants continue to remain dominant in Washington, and the country. We’ve seen a small increase in hospitalizations since our last newsletter, now up to 10.3 hospitalizations per 100,000 people.
As always, we urge you to take reasonable precautions, especially wearing a mask in crowded indoor areas, and hanging out with friends outdoors or in well-ventilated areas with some distance where possible.
🫤 The decline of American social trust
There’s a vigorous academic debate over the erosion of social trust in the US. Some theories, such as increasing ethnic diversity, have conflicting empirical studies for and against.
One aspect that seems more settled is general polarization, especially over what are often generalized as “cultural” issues (i.e. homosexuality and abortion). One 2016 study looked at data from 39 countries and found that the more opinions on these issues diverged, the less trusting people were of each other.
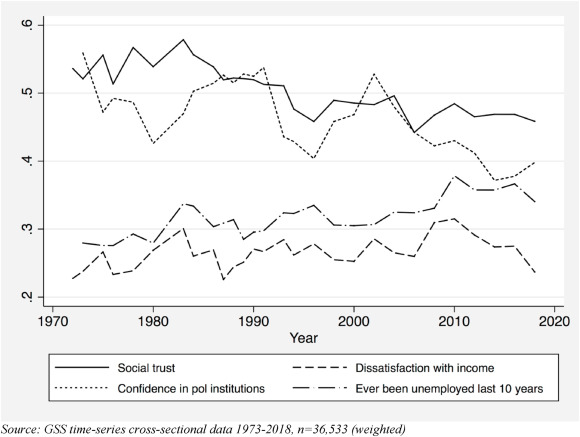
We can also learn more from a landmark 2021 empirical study of in the US (graph above), which determined the following individual factors reduced social trust:
- Becoming unemployed, also called “unemployment scarring”
- Confidence in political institutions
- Dissatisfaction with income, albeit marginally
When these measures are plotted over time, we see that social trust declined as the public learned the Iraq War was based on lies, or as more Americans dealt with the pain of unemployment from Wall Street crashing the economy in 2008. With both political parties captured by millionaires and billionaires, there’s been no real accountability for these devastating events in American life.
A related data point: a study found that Trump, who epitomizes a low trust viewpoint (i.e. “it’s all rigged, drain the swamp”), received a higher vote share in states with high military casualty rates in the 2016 presidential election.
Unfortunately, COVID appears to be another event that reduces social trust, like Iraq and the 2008 recession. While there is a lot that can be praised of our government’s response to COVID, like the record development and approval of vaccines or the enhanced unemployment and stimulus checks, there are also clearly some key problems.
The public health and pharmaceutical sectors, along with politicians, either ignorantly misled the public or lied about the power of vaccines to prevent infection, setting themselves up for backlash.
As Hopkins Medicine notes, the scientific community has long known coronaviruses and all types of viruses mutate frequently–it’s “neither new nor unexpected.” It’s one reason why sometimes the regular seasonal flu shot ends up not working–a variant emerges.
Faced with this scientific reality and precedent, why did our political and public health leaders mislead us about the power of vaccines?
On July 21, 2021, during a CNN Town Hall, Biden said: “You’re not going to get COVID if you have these vaccinations.”
Fauci said the same. He told the public last year, “When people are vaccinated, they can feel safe that they are not going to get infected.” Fauci and other officials said similar statements repeatedly.
Vaccine-skeptics have seized on these statements—which are now provably false—with one super cut now having 3.1 million views on Twitter. [A super cut is a series of very short video snippets spliced together to make a point.]
You could also take the example of masks. At the beginning of the pandemic, public health officials could have told the public something like, “Masks are in short supply, we are limiting the sale of them to hospitals and doctors until we can provide them for the general public.” Or they could have said, “We don’t yet have data on how effective masks are at preventing the spread of COVID.”
Instead, Dr. Fauci said the following in a March 2020, 60 Minutes interview:
“There’s no reason to be walking around with a mask. When you’re in the middle of an outbreak, wearing a mask might make people feel a little bit better, and it might even block a droplet. But it’s not providing the perfect protection that people think that it is. And often, there are unintended consequences. People keep fiddling with the mask, and they keep touching their face.”
These and other about-faces from the public health establishment has definitely damaged their credibility over the course of the pandemic. We need humble leaders who won’t lie to us or promise false things. If our leaders don’t know something with certainty, they should tell us so.
And if they mess up repeatedly, they should resign or be held accountable.
🤝 How to Build Social Trust
To build social trust, it helps to first look at countries around the world that are doing it right.
In polling, Nordic countries rank at the top. Academics investigating this ‘Nordic exceptionalism’ in the World Happiness Report in 2020 believe it’s the result of a virtuous cycle of interrelated factors, rather than a single one. They wrote,
“Does trust in institutions and other citizens create a fertile ground for building a welfare state model with extensive social benefits? Or does the welfare state model contribute to low crime and corruption, which leads citizens to trust each other more? Most likely, both directions of influence play a role, leading to a self-reinforcing feedback loop that produces high levels of trust in the Nordic region, and a high-functioning state and society model.”
Other studies have found evidence for the positive relationship between a welfare state, active labor market policies, and social trust. In the US, passage of the Affordable Care Act led to increased social trust.
Building a high-functioning welfare state or trying to heal the ‘culture war’ in America will take time, and probably a more strategic Left that can reverse the process of class dealignment.
More immediately, to respond to low levels of booster vaccination for COVID, we should focus on building trust in the public health world. That might mean a new, less polarizing, more honest face for the NIH than Dr. Fauci.
It should also mean investing in community health workers. Ed Wong explains in The Atlantic:
“America actually has an entire workforce that specializes in earning trust: community health workers. They’re hired for their empathy, their strong local ties, and their personal experience with hardship. Breanna Burke, a community health worker in Bristol, Tennessee, where she has lived since she was 3, told me that her job is to “get to the root cause of ongoing health issues,” with the understanding that a person’s circumstances constrain their choices. For example, she helped one of her diabetic clients plan a budget to keep their power on so they could keep their insulin cold; another time, she figured out that a patient whose pain wouldn’t stop had been sleeping on a hardwood floor for nine months, and contacted a local women’s club to raise money for a mattress.
When COVID hit, Burke provided people with emergency food supplies so they could weather quarantine in safety, and talked others through their hesitancy over getting vaccinated. She can do that because her nonjudgmental approach and shared life experience make her trustworthy—the secret to community health workers’ extraordinary effectiveness. In three randomized trials involving people living in poor parts of Philadelphia, Shreya Kangovi, a physician at the University of Pennsylvania, showed that people who see community health workers spend 66 percent fewer days in the hospital than those who receive usual care. In her research, Kangovi also found that every dollar invested in said workers returns $2.47 to the average Medicaid payer.”
Investing in community health workers would lead to improved COVID outcomes, and a healthier, more trusting society. We should do it!
🙏 COVID-19 Resources
- Order 8 free, at-home COVID tests (It doesn’t matter if you’ve placed a previous order through the same site.)
- Order 4 free at-home COVID tests (note: any single address can only be used one time)
- Additional option to order free at-home COVID tests (WA only)
- Find vaccines near you
- Testing locations
What do you think? Have any questions? Tweet us your thoughts @WACommAlliance.
Keep up on Washington’s latest COVID-19 trends, new research, and more through our Endemic newsletter.