Today, we’ll share everything you need to know about Paxlovid, the game-changing antiviral pill to treat COVID-19. But first, we’ll review the latest data on the current wave in Washington and the U.S. Hope everyone’s staying safe out there!
🙏 COVID-19 Resources
- NEW-ish! Order 8 free, at-home COVID tests (It doesn’t matter if you’ve placed a previous order through the same site.)
- Order 4 free at-home COVID tests (note: any single address can only be used one time)
- Additional option to order free at-home COVID tests (WA only)
- Find vaccines near you
- Testing locations
📊 Washington’s COVID-19 Weekly Snapshot
COVID cases 😷
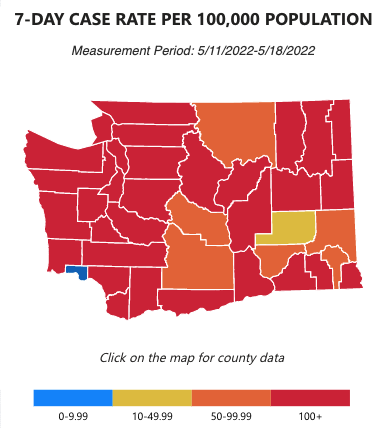
Wow. This week’s data graphic stands quite starkly against the same one in our last newsletter. The 100+ cases per 100 thousand people jumped from 20 to 31 counties (of Washington’s total 39). Just two weeks ago, 11 counties were in the 0-49.99 case range (in blue or yellow) but now there’s only 2.
Hospitalization rates 🏥
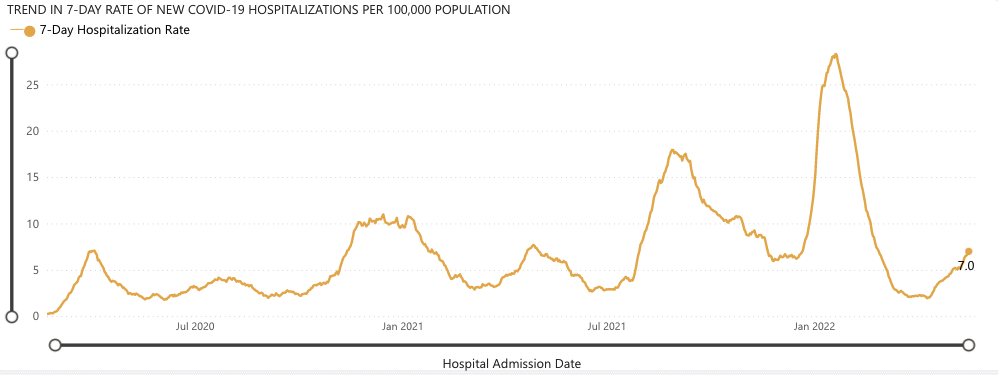
The Omicron BA.2.12.1 variant April 2022 wave has continued to increase, with hospitalizations now reaching an average of 7.0 per 100,000 people. Among the people in this wave are Gov. Jay Inslee and Lt. Gov. Denny Heck, who both unfortunately tested positive a week ago. They both had mild symptoms and are now recovering well.
Graph from New York Times
With high community spread in most of Washington, we advise you to take reasonable precautions, like wearing masks (N95s if you can!) indoors when there’s poor air ventilation and/or it’s crowded, and in elbow-to-elbow crowded outdoor areas (like, some sporting events where tons of strangers are quite literally sharing arm rests with each other and definitely at music festivals). Please stay safe out there!
For more detailed data, such as COVID-19 data by county, visit the WA DOH COVID-19 Data Dashboard.
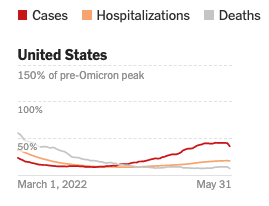
On the positive side, if we look at the country as a whole, we can see this wave plateauing and potentially beginning to decrease. We can also count our blessings—thanks to vaccinations, antivirals, and other improved treatments for COVID—that we have not seen death rates spike from this latest wave. (We know deaths lag behind cases and hospitalizations, but given the latest wave has been occurring for two months, we’d expect to have seen deaths increasing if they followed the pattern of previous waves.)
💊 Best practices for treating COVID with Paxlovid, the antiviral pill
Our greatest asset in the fight against COVID besides vaccines is now, undoubtedly, Pfizer’s drug Paxlovid. The antiviral pill reduces COVID’s ability to replicate and has been found in a clinical trial to reduce unvaccinated people’s risk of severe illness and death by 89%. That’s on par with vaccines themselves! There are other pills developed to treat COVID, but data suggest they’re far less effective.
Due to this, the FDA authorized (at the end of 2021) emergency use of Paxlovid to treat mild-to-moderate COVID patients who are 12-years-old or older and those at high risk of progressing to severe COVID (including hospitalization or death). Our federal government is purchasing the pills and distributing them free of charge!
The CDC encourages people speak to a doctor/provider to determine if they’re eligible for Paxlovid. A map from the federal government shows locations for COVID medical visits, including ‘Test to Treat’ locations, that pair testing and treatment.
But, in case it helps you (and your community) in advance, here is the CDC’s list of conditions that put one at greater risk of severe COVID:
- 65 years or older
- Occupational or location-based hazards to health
- Racial and ethnic minority groups due to higher chronic health conditions
- Cancer
- Chronic kidney disease (if severe kidney disease, Paxlovid is not recommended)
- Chronic liver disease
- Chronic lung diseases
- Cystic fibrosis
- Dementia or other neurological conditions
- Diabetes (type 1 or type 2), Disabilities (such as ADHD, cerebral palsy, and others)
- Heart conditions
- HIV infection
- Immunocompromised condition or weakened immune system
- Mental health conditions (such as depression)
- Overweight and obesity
- Physical inactivity
- Pregnancy
- Sickle cell disease or thalassemia
- Smoking (current or former)
- Solid organ or blood stem cell transplant
- Stroke or cerebrovascular disease
- Substance use disorders
- Tuberculosis
Since 2.8 million doses of Paxlovid have been ordered but only 1 million doses have been administered, it’s likely that doctors will be generous—not overly strict—with their prescriptions to help treat COVID.
The key with Paxlovid is to not delay. Treatment must be started within the first few days of COVID symptoms to be effective.
The CDC did identify a ‘rebound’ phenomenon with Paxlovid where, after the 5-day treatment course, COVID symptoms can return. However, the symptoms are milder and the CDC hasn’t seen any evidence of hospitalization following treatment, so it still excels at its job.
From our research, the greatest problem with Paxlovid is it’s likely not getting to people who need it the most! As we’ve written about before, many working class and marginalized people facing higher risk of severe COVID don’t use healthcare as much due to cost, time, distrust, and other barriers.
With medical bills being the #1 reason for bankruptcy in the US, this isn’t surprising.
Until we adopt a single-payer Medicare-for-All system that ensures all of us, regardless of our income or race, receive high-quality healthcare, we will keep seeing shameful disparities and dysfunction in healthcare.
What do you think? Have any questions? Tweet us your thoughts @WACommAlliance.
Keep up on Washington’s latest COVID-19 trends, new research, and more through our Endemic newsletter.