We’re pleased to present you with Grab Bag Edition #2. Some of you have sent in excellent questions and we want to be sure we provide answers to them. Plus, we wanted to give you a quick overview of monkeypox, given recent outbreaks.
🙏 COVID-19 Resources
All past newsletters have had these resources but we’re bringing it back up to the top due to the monkeypox vaccinations available in King County. Whether above or below, we’ll always keep this resource list around! Here’s what’s available:
- King County monkeypox vaccination page
- Order 8 free, at-home COVID tests (It doesn’t matter if you’ve placed a previous order through the same site.)
- Order 4 free at-home COVID tests (note: any single address can only be used one time)
- Additional option to order free at-home COVID tests (WA only)
- Find vaccines near you (especially for those newly-eligible kiddos!)
- Testing locations
📊 Washington’s COVID-19 Weekly Snapshot
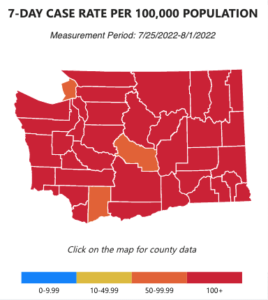
COVID cases 😷
Hospitalization rates 🏥
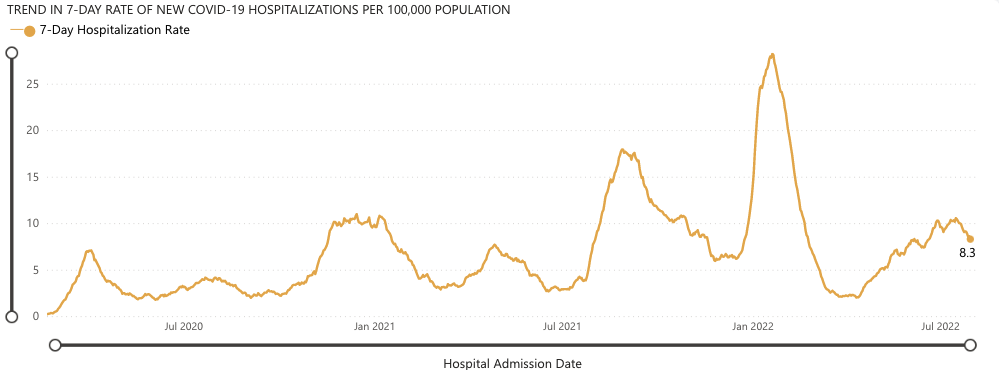
We are in the long plateau of Omicron’s variants. As a recent CNN headline put it, “The US is on a COVID plateau, and no one’s sure what will happen next.” Nationally, we’re seeing 40,000 people hospitalized and 400 deaths per day on average. Fortunately in Washington, hospitalizations are beginning to slightly trend downward from a high at the beginning of July.
It’s not clear what will happen next—there are new Omicron variants on the horizon, like BA 4.6 and BA 2.75. Otherwise, plans are still in motion for Omicron-specific boosters to be ready this fall.
As always, we urge you to take reasonable precautions: Wearing a mask in crowded indoor areas (including busy grocery stores), and hanging out with friends outside or in well-ventilated areas with some distance where possible.
🛍 Grab Bag #2: Vaccine safety, preventing spread at home, and the monkeypox
Thank you, again, dear readers, for sending in your questions! We know if you have a question, there are bound to be many more people who have it as well. Be sure to subscribe to these e-newsletters so you get them on time!
🫀 The safety of COVID-19 vaccines for kids & heart disease: What do we know?
It’s been well established that your risk from COVID-19 worsens the older you are. We want all children to be healthy and safe, but children can still catch COVID-19 and it’s nothing to trivialize: Since the beginning of the pandemic, over 140,000 American children (ages 0-17) have been hospitalized with COVID-19 and 1,734 have died, according to the CDC. Children who catch COVID-19 can also have health impacts beyond the virus, such as induced diabetes.
One age group we’ve had questions about in particular are babies, and whether they can catch COVID. Based on studies, we know that babies can catch COVID, usually with mild symptoms (fever or nasal congestion, for example) or are asymptomatic.
For the reasons above, COVID-19 vaccines for children (6 months and older) have been developed and approved by the FDA. You may be wondering, are there side effects or dangerous health effects associated with these vaccines?
There is one RARE but known side effect of mRNA vaccines: myocarditis (inflammation of the heart muscle) that particularly affects teenage boys and young men.
Rare is important to emphasize. According to the CDC and multiple studies, the rate of this side effect is around 70 cases per 1 MILLION doses. The rate of incidence (AKA frequency) was highest among MEN aged 18-25 after receiving the second dose, according to a large study in the US by The Lancet. This finding has been confirmed in other studies from Israel, Canada, and others. There have been hospitalizations from myocarditis related to the vaccine, but critically, no deaths.
To sum up: while the risks associated with catching COVID-19 are lower for children, they are still very serious. And while teenage boys and young men have a higher risk for a side effect to the vaccine, many studies have established that the benefits far outweigh the risks (see multiple studies by the CDC and by independent scientists).
✋ How to limit the spread of COVID-19 in shared living situations
If you catch COVID-19 and live with family or housemates, you’ll want to avoid spreading the virus, even if your housemates are vaccinated. The vaccines generally do not prevent infection from recent variants, and you’ll want to save your housemates from getting sick (even if the risk of severe illness is low). We suggest that:
- The person who is sick isolate in their room while testing positive, and wear an N95 mask outside of their room. When using the bathroom, wash hands thoroughly!
- Other housemates also wear N95 masks when in the same room as the sick person to further significantly decrease odds of infection.
- The whole household take steps to increase ventilation, like opening windows and/or running fans while someone remains positive for COVID-19.
🦠 About Monkeypox
Monkeypox virus (MPV) is a virus that originates in Africa and is currently seeing its first-ever sustained global transmission. Be on the lookout for its symptoms: fever, headache, body aches, swollen lymph nodes, exhaustion, lesions (which start off looking like blisters or pimples), and skin rashes. While some strains in Africa can cause death, the strain circulating globally is non-lethal and most people recover within 2-4 weeks. That said, it can be very painful.
From what we know of the global strain, it is primarily spread through close skin-to-skin contact [including animals] and/or skin-to-mouth contact.
For that reason, spread is primarily through sexual contact. The most infection-prone type of sexual contact has always been the rectum, because of the way it easily tears. This is true across almost all sexually-transmitted diseases—which is a large reason we’re seeing disproportionate impact to the LGBTQ+ community, particularly gay men, at the beginning of a mainly-sexually-transmitted spread. Of course, not only gay men have rectal intercourse, so keep this factoid in mind regardless of sexual orientation!
Monkeypox can also spread through contact with contaminated surfaces, like bedding, or through aerosols (small liquid droplets from coughing, sneezing)—but these methods of spread, based on our current knowledge, are far less common.
So far, the virus is concentrated almost entirely with males that have male-to-male sexual contact. According to the CDC’s technical report: “Of the 1,383 patients with information on sex assigned at birth, 99.1% were assigned male sex (13 assigned female sex). Among the male patients with information on sexual activity, 99% (n=624) reported male-to-male sexual contact.” To be clear, this does NOT mean that straight people or lesbian folks can’t get monkeypox. They can, and have.
This national data is backed up by Tuesday’s newsletter from King County (where the bulk of our state’s cases are located) Public Health: “To date, all of the people diagnosed with monkeypox in King County have been among men* who reported close intimate contact with other men, sometimes with anonymous partners. *This includes people who may identify as non-binary, gender queer, or transgender.”
However, public health officials say that the virus could expand to include more people of all sexes and sexual orientations.
What should we do? To start, EVERYONE should be careful about having sex with new partners during this outbreak. The Associated Press recently reported hopes that the virus can still be contained, writing “Except for Africa, there is no sign of sustained monkeypox transmission beyond men who have sex with men, meaning that stopping spread among that group could effectively end the outbreak.”
The federal Department of Health and Human Services has already shipped out 620,000+ vaccines focused on reaching high-risk individuals (gay and bisexual men). Public health officials in King County are distributing the vaccines directly to providers that serve individuals at risk, to the Sexual Health Clinic at Harborview, and to community access points to reach underserved individuals. We searched for a statewide list of monkeypox vaccination locations, or at least locations in metropolitan hubs across the state, but found no such reliable resource for either.
If you have any potential symptoms, we encourage you to contact your health provider or local public health department immediately. The monkeypox vaccine (usually JYNNEOS) is only recommended WITHIN 4 DAYS of the EXPOSURE DATE, but not after that time period while infected.
We encourage individuals and communities at highest risk, such as gay and bisexual men, to seek vaccination.
People are not considered fully vaccinated until their second shot, which most advisories have happening 28 days after the first shot, largely due to stockpile limitations. People who have been vaccinated for smallpox—which stopped being required after the ‘70s–are considered vaccinated for monkeypox. Those who receive JYNNEOS are effectively in the clear for smallpox, too, because the strains are very closely related.
We also encourage those at highest risk to take precautions based on our knowledge of how the virus spreads, such as reducing close physical contact with unvaccinated and especially newly-met individuals, especially if they have any MPV symptoms, until the outbreak is more contained.
David Mack, a gay journalist at Buzzfeed, recently wrote about how the World Health Organization has urged men who have sex with men to reduce partners and reconsider sleeping with new partners.
As a public, we should also be vigilant against a potential increase in hate crimes against gay and transgender men due to monkeypox. And critically, our municipal, state, and federal elected officials should be funding vaccination outreach efforts while the virus is still in early weeks of spread; Now is the time for collective and public investment, not later. Being proactive is the name of the game when it comes to new virus containment. If we get serious now, we’ll have a decent shot at containing monkeypox.
What do you think? Have any questions? Tweet us your thoughts @WACommAlliance.
Keep up on Washington’s latest COVID-19 trends, new research, and more through our Endemic newsletter.