Friends— President Biden stirred up a small controversy last week when he said “the pandemic is over” in a 60 Minutes interview. In the next sentence, he clarified, “COVID is still a big problem, and we’re still doing a lot of work on it, but the pandemic is over.” Is Biden right? In this Endemic, we’ll discuss what it means for a pandemic to be “over” and what we can predict for COVID into the future.
📊 Washington’s COVID-19 Weekly Snapshot
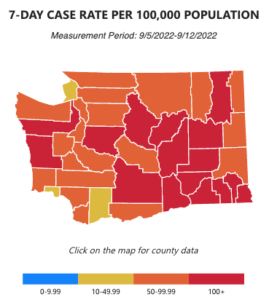
COVID cases 😷
Hospitalization rates 🏥
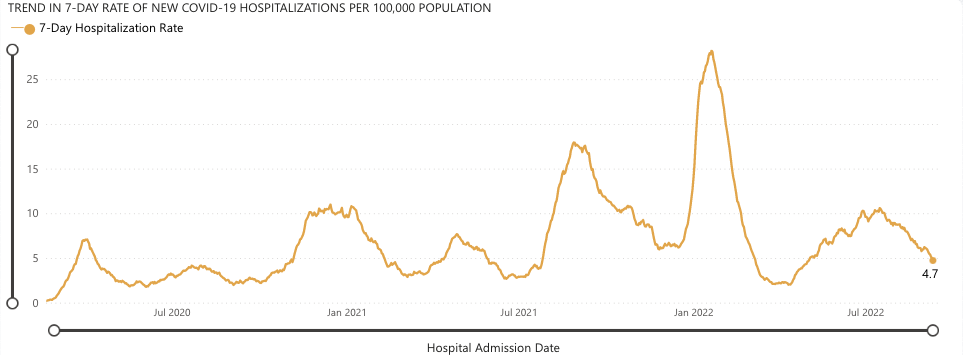
Hospitalizations from COVID continue to drop which is welcome news. We’re down to 4.7 cases per 100,000 people, which is about half of what it was in July. But we need to keep up our guard, as the rate of spread is still considered moderate to high in most of the state. We continue to urge that you wear an N95 mask in crowded indoor areas and take precautions. And get those new and improved boosters.
Washington is also making news because state employees just negotiated a contract to receive $1,000 bonuses for getting boosted. Doesn’t sound bad at all—yet another reason why unions are great.
🤷♀️ When is a pandemic ‘over’?
In the first emails of our Endemic newsletter, we shared our viewpoint that we’re indeed still in a pandemic, but beginning to undergo a transition to an endemic phase, meaning the virus becomes a regular presence in human life, similar to the flu. There’s no official marker for when a virus transitions from a pandemic to endemic, but most scientists agree it’s when a virus becomes predictable.
The flu is a great example of a truly endemic virus: It has predictable seasonality and the deaths from it are generally stable from year to year. Let’s compare COVID to the flu on a couple of metrics.
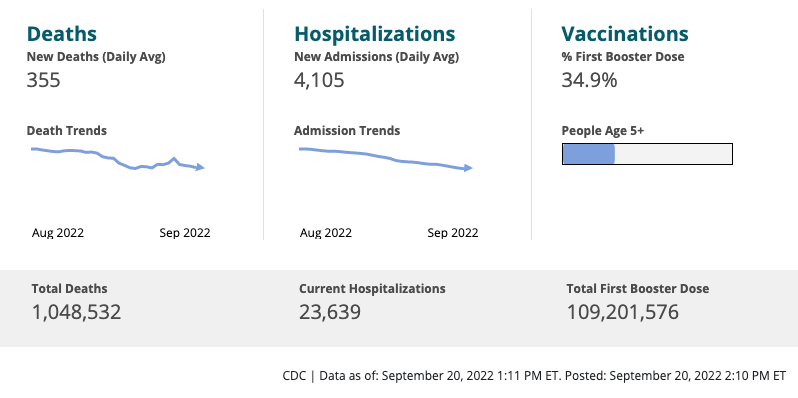
Deaths
The CDC estimates that an average of 36,000 people died of the flu each year over the past decade (10 years). If the current rate of COVID’s 355 daily deaths continued, we would see around 130,000 deaths a year.
When considering the official death toll from COVID, it’s also important to take into account how it’s counted. If you died principally from another disease, while also being sick with COVID, your death is counted as a COVID death. COVID often worsens other conditions, but the nuance is important.
Dr. Bob Wachter, the chair of the University of California San Francisco’s department of medicine, told NBC he thinks about half of all recent COVID deaths would fall under the “with” not “from” category.
So with that estimate, we’re closer to 70,000 deaths from COVID a year.
Some scientists believe that with current trends from COVID, it’s possible it will become more similar to the Flu’s 36,000 deaths a year. In another interview with NBC, Dr. Chris Murray, the director of the Institute for Health Metrics and Evaluation at UW, said, “It would not surprise me if we have a similar magnitude of deaths from COVID as we do from flu.”
Seasonality
For the most part, scientists agree that there has been no seasonal trend with COVID. Surges in the virus have been associated with when variants emerge as opposed to seasons.
Predictability
Usually, endemic viruses like the Flu do not have extreme surges in death or illness from year to year. While COVID has been on a plateau or slightly downward trend for the past month and a half, the virus is still unpredictable. There are already new variants of concern, such as Omicron’s BA.2.75.2 or BA.7 which can more strongly evade immunity.
We can’t say with certainty if these variants will cause large waves or a series of more predictable, smaller waves.
But together, we do have the ability to make the virus much more predictable. The higher the rate of the spread, the higher the rate of new mutations and variants. If we tamped down spread through nasal vaccines, robust ventilation, and masking in crowded indoor areas, we would see fewer new variants. Whether that’s enough for COVID to truly become “predictable” similar to the flu, is unknown.
The big picture
We disagree with Biden; The pandemic isn’t over because the virus isn’t predictable enough yet. The next few months will be very revealing: Will we see new variants surge or current trends continue?
At some level, COVID is also about the tradeoffs we as a society make around individual freedom and personal choices versus collective responsibility. The prospect of 36,000 deaths a year from COVID is awful. But for some perspective, the CDC estimates around 140,000 deaths a year from excessive alcohol use.
If COVID hawks want the public to adopt greater concern over COVID, it will have to be through smart and effective persuasion rather than shaming or ridiculing people. And it means listening to, and maybe compromising around, the real concerns and tradeoffs people have around COVID, whether it’s economic impacts or effects on our children’s education. It means listening to the many communities of color that have experienced systemic racism within the healthcare system and are rightly skeptical of it, and doing tangible things to respond such as investing in Community Health Workers.
We should even listen to the people who believe COVID is a plot by Bill Gates to make money from vaccines and Big Pharma. No really, in the sense, these ideas don’t come out of the void. In 2020, we saw around 70,000 deaths from the opioid epidemic. We know that Big Pharma colluded and bribed doctors to overprescribe addictive painkillers. People generally aren’t dumb—they understand that profit motives drive a huge amount of our healthcare system, and that corruption is common. It’s not too much of a leap from there to Bill Gates conspiracies.
At the end of the day, COVID is wound up in the broader problems our society faces. The labor organizer and author Jane McAlevey, titled one of her books, “No Shortcuts: Organizing for Power in the New Gilded Age”. We think that same philosophy applies to COVID. There aren’t any “easy shortcuts” to an effective, holistic response to COVID when a society becomes as distrustful, profit-centric, and fragmented as ours.
In her book, McAlevey makes the case that mobilizing a small cadre of activists is no substitute to real organizing, which is about bringing new people (especially when we may not hold all the same progressive beliefs) into a movement, a union, a community group, a campaign, and so on. We agree.
🙏 COVID-19 And Monkeypox Resources
Whether above or below, we’ll always keep this resource list around! Here’s what’s available:
- Use the Department of Health (DOH) Vaccine Locator tool for
Omicron Boosters! - King County monkeypox vaccination page
- Order 8 free, at-home COVID tests (It doesn’t matter if you’ve placed a previous order through the same site.)
- Order 4 free at-home COVID tests (note: any single address can only be used one time)
- Additional option to order free at-home COVID tests (WA only)
- Find vaccines near you (especially for those newly-eligible kiddos!)
- Testing locations
- DOH’s Care Connect (1-800-525-0127) for COVID-positive people’s free assistance on grocery delivery, medication delivery, and help with other core needs.
The DOH has told the public that demand is likely to exceed supply for the first few weeks, so maybe take that into account. For example, if you’ve recently had COVID, then you have some recent natural immunity, and therefore could wait 2-4 weeks (conservatively) before getting your booster.
What do you think? Have any questions? Tweet us your thoughts @WACommAlliance.
Keep up on Washington’s latest COVID-19 trends, new research, and more through our Endemic newsletter.