Friends— We wanted to let you know we’ve certainly been paying attention to your selections in our sign-up form for “Endemic.” A lot of you said you’re most interested in learning about long-COVID findings! So today, we’ll dive into the treacherous and confounding topic after looking at the alarming COVID trends in Washington state first.
🙏 COVID-19 Resources
- NEW! Order 8 free, at-home COVID tests (It doesn’t matter if you’ve placed a previous order through the same site.)
- Order 4 free at-home COVID tests (note: any single address can only be used one time)
- Additional option to order free at-home COVID tests (WA only)
- Find vaccines near you
- Testing locations
📊 Washington’s COVID-19 Weekly Snapshot
Hospitalization rates 🏥
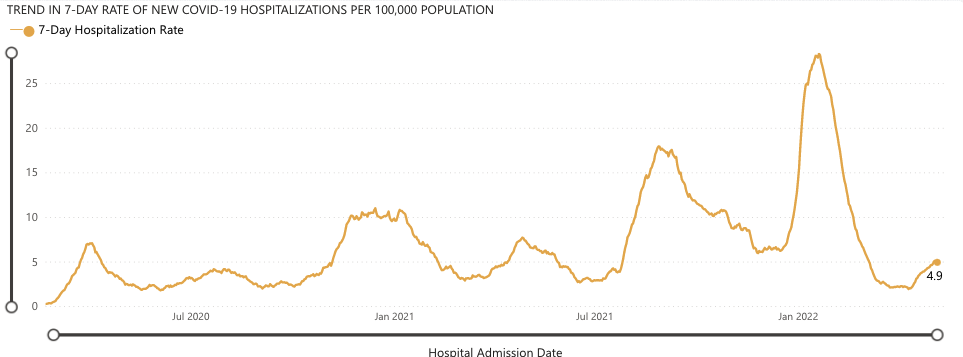
We are definitely in a wave from the Omicron BA.2.12.1 variant.
May 7th is the latest data point from Washington state’s Department of Health (DOH), with an average of 4.9 hospitalizations per 100,000 people. For reference, it was around 1.9 at the beginning of April.
On the positive side, the rate of increase in hospitalizations is not as high as it was in previous waves. That’s due to reduced severity of new variants, immunity built up from vaccines, immunity built up from catching COVID previously (although the more one catches COVID, the more the negative symptoms present), and availability of antiviral treatments.
Given the high community spread in most of Washington, we advise you take reasonable precautions like avoiding crowded places when possible, and wearing masks (N95s if you can!) in indoor areas with people and/or in places of poor air ventilation.
For more detailed data, such as COVID-19 data by county, visit the WA DOH COVID-19 Data Dashboard.
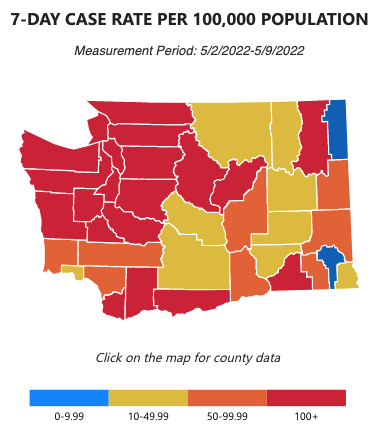
COVID cases 😷
🦠 A Short Explainer for Long COVID
“Long COVID” is a term used to describe the experience of COVID-19 after-effects where often severe symptoms last months or years. It’s estimated to affect one in three people who contract COVID. With over 60% of Americans having done so, we can estimate that around 20% of the general population is experiencing some form of long COVID. And, well, that’s a lot of people! (66,480,730 to be exact.)
Long COVID has been especially difficult for scientists to study because it can’t be tested for yet, requires “longitudinal” (as in, months- to years-long) studies, and because its symptoms overlap with many other diseases. As such, it’s difficult for everyday people to suss out if they’re even experiencing long COVID symptoms, much less report it. But studies rely on people who self-report. This generally leaves out lower-income and marginalized people who both face higher rates of COVID-19 and don’t use healthcare as much due to cost, time, distrust, and even more barriers.
With that said, here’s what we know: A representative survey of people who self-reported long COVID symptoms in the UK found the most common symptoms were:
- fatigue (51%)
- shortness of breath (33%)
- loss of sense of smell (26%); and
- difficulty concentrating (23%).
Another study in the US found the most common symptom was difficulty breathing, but symptoms can be wide-ranging, including heartbeat abnormalities and anxiety. The graph below shows the full spread of diagnoses:
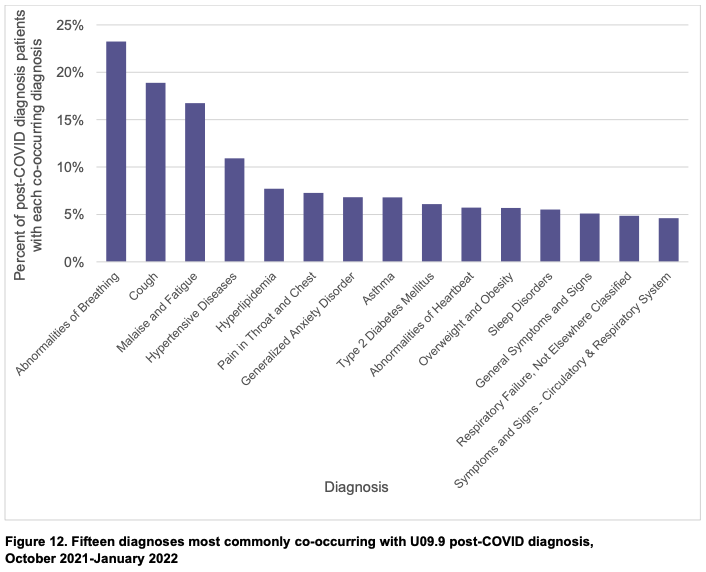
Generally, the more severe a patient’s COVID case was, the more likely they are to have long COVID.
In the UK, one study found people who had to be hospitalized for COVID experienced the equivalent of 20 years of mental aging or losing about 10 IQ points.
But long COVID is not limited to severe acute cases.
A US study published this week found that 75% of people experiencing long COVID had not been hospitalized. This study, which looked at 78,252 long COVID patients with private health insurance in the US and is one of the largest of its kind, had a number of other key findings:
- 60% of the long COVID patients were female. One researcher hypothesized this is due to the same biological differences that also happen to make women more likely to experience autoimmune disorders.
- 30.7% of the patients had no reported pre-existing condition even though pre-existing conditions, like diabetes or chronic kidney disease, make you more likely to experience long COVID.
- People ages 36-50 were most likely to experience long COVID.
- Long COVID patients were much more likely to experience muscle disorders (myopathies) than in the same population prior to COVID.
From another study this year, we’ve also learned that some long COVID patients have symptoms produced by a reactivation of an otherwise dormant Epstein-Barr virus—a common virus that most people catch at some point in life, especially during childhood.
It’s clear that scientists still don’t fully understand the mechanism by which long COVID affects the body, and that more research is needed. On the positive side, there are some promising leads on the ways to prevent and treat long COVID:
- Vaccines help! A UK study found that getting doubly-vaccinated reduced the odds of contracting long COVID by 41.1% for the Delta variant, compared to not being vaccinated. Right now, there’s more people in Washington state with only one vaccination (81.8%) than there are those with two (74.4%). In the same study, people who had a breakthrough case of Delta and then went on to receive a booster had their risk of developing long COVID cut in half.
- A very recent and small study by the University of California found Pfizer’s COVID antiviral drug, Paxlovid, helped reduce the symptoms of long COVID patients. The drug is not yet approved by the FDA, and we can expect more studies to follow.
- A long COVID treatment clinic found that exercise and/or antidepressants help treat long COVID for many patients.
The same University of California clinic also shared the most hopeful news we’ve come across while researching long COVID:
“’In general, these patients get better over time,’ [said Mark Avdalovic, a specialist in pulmonary and critical care medicine and director of the clinic]. The first 15 patients seen at the clinic were all experiencing fatigue and shortness of breath. They saw their symptoms improve after seven weeks of pulmonary training or exercise to strengthen the lungs. Participants improved on the six-minute walk test, which measures how far someone can walk in six minutes, and their cardiovascular response.
‘With about three-fourths of our patients, things eventually come back to either normal or near-normal for them. But it’s just that for some, it takes a long time,’ Avdalovic said.
We hope you’ve learned some new things and gained a better understanding of long COVID. Stay safe out there!
What do you think? Have any questions? Tweet us your thoughts @WACommAlliance.
Keep up on Washington’s latest COVID-19 trends, new research, and more through our Endemic newsletter.